Progress Note Overview
Steps
Create a note from the calendar
Click Scheduling > Click the appointment > Notes tab> Create a Progress Note

Clicking on a completed appointment brings up a dialog with additional details regarding the appointment as well as related notes and billing items. The Notes tab of this dialog provides links to note that may be related to the session, including the Progress Note.
Note: All Progress Notes should be done in SOAP format
SOAP notes include four headings that correspond with each letter of the acronym:
Subjective
Objective
Assessment
Plan
Diagnosis

The Diagnosis section will automatically populate a DSM-5 diagnosis code and description based on the information entered in the client's Treatment Plan developed by the Rehab Specialist.
Current Mental Status

Progress Notes contain a full Current Mental Status exam. Use our one-click autofill options (All Normal or All Not Assessed) to simultaneously fill each of the fields, click in each field to select from a list of common responses, or enter your own information in each field.
Symptom Description and Subjective Report
This section is for subjective reporting of how your client says they are feeling during the session and what they report about their current symptoms. It can also contain information gathered from family members
The information in this field may answer questions such as, "How is the person is doing?", "What is the client's perspective about the problem?", or "What is the client’s opinion of the therapeutic intervention or service?" In this field, you may also document any information about the client given to you by someone else that you cannot verify but has an impact on the session or services.
Objective Content
This part of your SOAP note should be made up of physical findings gathered from the session with your client.
There are two types of objective data: the provider’s observations and outside written materials. This is the section to document that which can be seen, heard, smelled, counted, or measured. You can document observations such as the mood and affect of the client here as well.
The Objective Content field is also where you can document specific information about conversations or interventions used during the session.
Note: This section should consist of factual information that you observe and not include anything the patient has told you.
Interventions Used
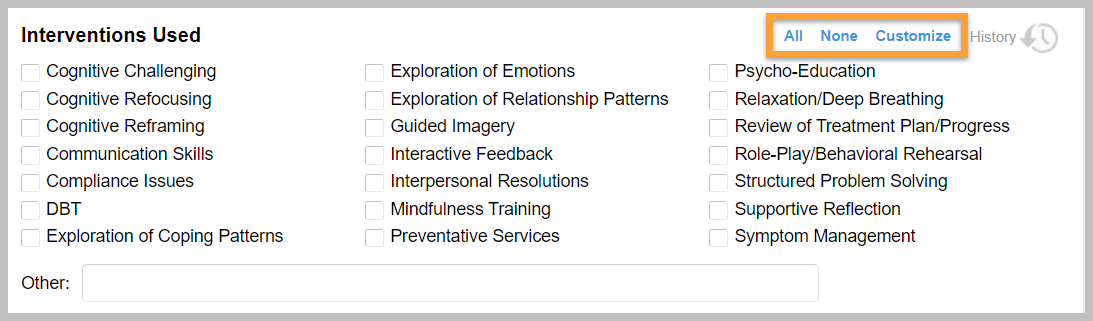
Select the appropriate checkboxes to document the interventions utilized during the session. This can assist with ensuring that you meet documentation requirements for some payers by clearly delineating specific therapeutic approaches.
Your interventions list is customizable to make it easy to list the interventions you use most frequently. Click Customize to add or delete custom interventions.
Treatment Plan Progress
Document progress towards each of your treatment plan objectives. Click each Progress field to select from a list of common responses, or enter your own assessment. This enhances the closed-loop documentation approach, as you specifically link interventions in the session to objectives identified on the client's Treatment Plan.
Additional Notes / Assessment
Document the client’s response to your interventions, your assessment of client functioning and progress, medical necessity for ongoing treatment, or your case conceptualization.
Plan, Recommendation, and Prescribed Frequency of Treatment
The last section of your SOAP note should outline your plan for next steps to treat the patient.
It can include short and long term goals for your patient and be as specific as what you plan to work on in the next session or as general as your expectations for the duration of treatment.
Sign and Save
Once you have completed your Progress Note for the session, select the Sign this Form checkbox to electronically sign the note and click the Create Note button. Electronic signatures are captured in accordance with appropriate requirements. Multiple factor authentication is required to identify the user signing the note. The application automatically captures the timestamp for the signature as well. Electronic signatures cannot be edited or modified.

Last updated